
Are you preparing for childbirth but worried about potential complications? Cephalopelvic disproportion (CPD) is a condition that every expectant parent should understand.
CPD occurs when a baby’s head is too large to pass safely through the mother’s pelvis during vaginal delivery. This common obstetric challenge affects approximately 1 in 250 pregnancies and is a leading indication for cesarean deliveries worldwide.
For expectant parents, understanding CPD can be crucial for birth preparation and reducing anxiety.
Knowing the signs, risk factors, and management options empowers you to have informed discussions with your healthcare provider and make confident decisions about your delivery plan.
Join us as we explore everything you need to know about CPD and how to handle this potential childbirth challenge.
What is Cephalopelvic Disproportion?
Cephalopelvic disproportion (CPD) is a condition where a baby’s head or body is too large to pass through the mother’s pelvis during childbirth safely.
It occurs when there’s a mismatch between the size of the fetal head and the maternal pelvic dimensions.
While normal birth involves the baby gradually descending through the birth canal as contractions dilate the cervix, CPD prevents this progression, causing labor to stall despite strong contractions.
Unlike typical births, where the baby’s head molds to fit the pelvis, CPD creates a physical obstruction that cannot be overcome naturally.
This condition requires medical intervention, typically a cesarean delivery, to ensure the safety of both mother and baby.
Causes of Cephalopelvic Disproportion
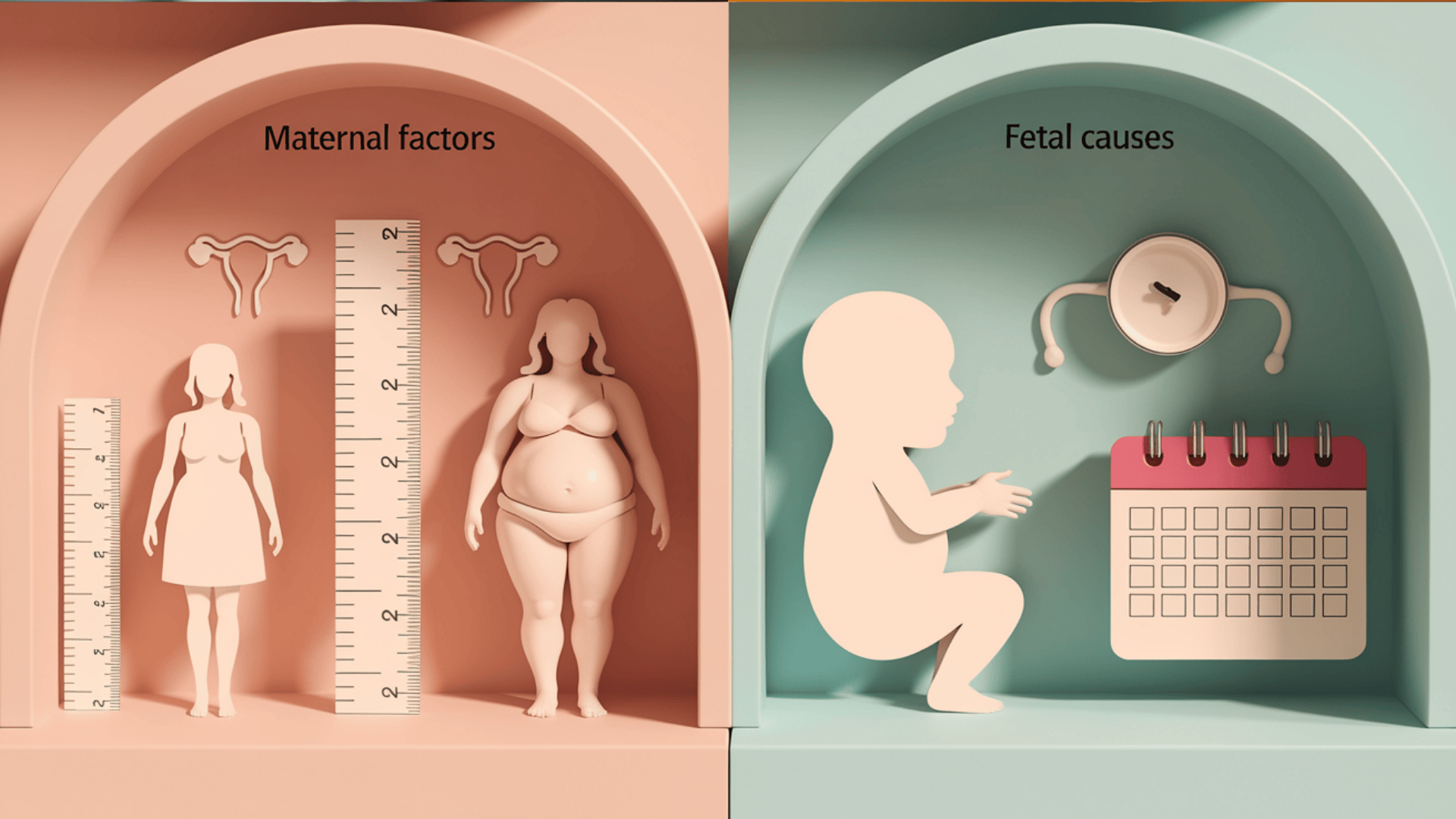
Here are the causes of cephalopelvic disproportion, a condition that occurs when a baby cannot safely pass through the mother’s pelvis during childbirth due to size incompatibility.
Maternal Pelvic Factors
- Naturally small or irregularly shaped pelvis
- Previous pelvic fractures or trauma
- Abnormalities from conditions like rickets
Fetal Factors
- Macrosomia (birth weight exceeding 8.8 pounds)
- Link to maternal diabetes
- Post-term pregnancies
Positional Issues
- Unusual fetal positioning
- Occiput posterior (face-up) presentation
- Shoulder presentations
- Mechanical challenges, even with adequate pelvic dimensions
Genetic and Developmental Factors
- Inherited tendencies toward larger head circumferences
- Specific skeletal structures affecting fit
Maternal Age Considerations
- Adolescent mothers with potentially immature pelvic development
- Women with android (male-type) pelvises
- Narrower front-to-back pelvic dimensions
- Increased obstruction likelihood during delivery
Risk Factors for Cephalopelvic Disproportion (CPD)

Cephalopelvic disproportion (CPD) occurs when a baby’s head or body is too large to pass through the mother’s pelvis during childbirth. While rare, several maternal, fetal, and historical factors can increase the risk of CPD.
Understanding these risks can help guide prenatal care and delivery planning.
| CATEGORY | RISK FACTOR | BRIEF EXPLANATION |
|---|---|---|
| Maternal Factors | Age >35 (first-time moms) | Higher risk of complications and reduced pelvic flexibility |
| Short stature ( | Often linked to a smaller pelvic outlet | |
| Obesity | Increases macrosomia risk and complicates assessment | |
| Fetal Factors | Post-term pregnancy (>40 weeks) | Baby continues growing, increasing in size |
| Male baby | Typically larger head circumference | |
| Abnormal position (e.g., posterior) | Makes vaginal delivery more difficult | |
| Obstetric History | Previous CPD | High likelihood of recurrence |
| Difficult past delivery | May indicate undiagnosed CPD | |
| Prior C-section (failure to progress) | Often a sign of unrecognized CPD |
Recognizing the risk factors for CPD allows healthcare providers to monitor pregnancies more closely and consider early interventions when needed.
While not all cases of difficult labor are due to CPD, awareness of these indicators supports better outcomes for both mother and baby.
Signs and Symptoms

Cephalopelvic disproportion often isn’t diagnosed until labor begins. Certain signs during labor may suggest CPD is present and interfering with vaginal delivery.
1. During Pregnancy
During pregnancy, few definitive symptoms indicate CPD before labor begins. However, healthcare providers may note a baby that measures large for gestational age during routine ultrasounds or fundal height measurements.
Some women experience persistent fetal positioning high in the abdomen (high floating head) near term, as the baby’s head cannot descend into the pelvis. Excessive discomfort with fetal movement in late pregnancy, particularly in the lower abdomen, may also indicate potential space constraints.
2. During Labor
The most obvious signs emerge during labor. Failure to progress despite adequate contractions is the hallmark symptom, with cervical dilation stalling despite hours of regular contractions. The baby’s head may remain high or fail to engage in the pelvis.
Prolonged first or second stage labor often occurs, and molding (reshaping) of the baby’s head may be excessive but still insufficient for passage. Mothers may experience intensifying back pain that persists despite changes in position.
3. Warning Signs for Healthcare Providers
Healthcare providers watch for several clinical indicators. Arrested descent of the fetal head despite adequate pushing efforts is concerning. Fetal heart rate abnormalities may develop, suggesting distress from prolonged compression.
Excessive caput succedaneum (scalp swelling) may form as the baby’s head presses against the cervix or pelvis unsuccessfully. The mother may develop severe exhaustion, fever, or signs of infection with prolonged labor. Pelvic examinations might reveal significant overriding of the fetal skull bones (severe molding) without progress.
Diagnosis of CPD

Diagnosing cephalopelvic disproportion involves multiple assessment approaches.
Prenatally, healthcare providers evaluate risk factors through physical examinations, measuring maternal height and pelvic dimensions, and tracking fetal growth via ultrasound.
They assess fundal height measurements at routine visits to identify potential macrosomia. During labor (intrapartum), diagnosis becomes more definitive, with a focus on labor progression patterns.
Key indicators include failure to progress despite adequate contractions, inability of the fetal head to descend into the pelvis, and excessive molding of the fetal head without advancement—various imaging techniques aid diagnosis, though their use varies.
Ultrasound helps estimate fetal weight and position, while traditional X-ray pelvimetry has largely been replaced by clinical assessment and CT pelvimetry in more complex cases. MRI provides detailed pelvic measurements but is rarely used routinely.
Diagnosis ultimately combines clinical findings with appropriate imaging, as needed.
Treatment and Management Options

Managing CPD focuses on ensuring a safe delivery for both mother and baby. Treatment plans typically depend on the severity and timing of the diagnosis during labor.
1. Labor Management Strategies
When CPD is suspected but not confirmed, healthcare providers employ several strategies to manage the condition. These include allowing more time for labor progression, encouraging maternal position changes to optimize pelvic dimensions, and ensuring adequate hydration.
Continuous fetal monitoring assesses the baby’s tolerance of labor. Oxytocin augmentation may strengthen contractions if they’re inadequate. Specialized positioning tools, such as peanut balls, can help maximize pelvic space.
This approach is most effective in borderline cases where some progress is being made and the maternal-fetal status remains reassuring.
2. Assisted Vaginal Delivery Possibilities
In cases of mild disproportion where the baby’s head has descended into the pelvis, assisted vaginal delivery might be possible. Vacuum extraction or forceps can provide additional force to overcome moderate resistance.
These interventions require careful patient selection—the baby must be properly positioned and engaged in the pelvis. The provider evaluates station, position, and estimated fetal size before attempting instrumental delivery.
This approach balances avoiding unnecessary surgery while ensuring safety when complete obstruction isn’t present.
3. Cesarean Delivery Indications and Process
Cesarean delivery remains the definitive treatment for true CPD. Indications include arrested labor despite adequate contractions, fetal distress, or clear clinical evidence of significant disproportion.
The procedure may be planned if diagnosed before labor or performed emergently if discovered during labor. A low transverse uterine incision is typical, with standard postoperative care focusing on pain management, infection prevention, and mobility encouragement.
Recovery typically takes 4-6 weeks, with counseling about delivery options for future pregnancies.
Recovery After CPD-Related Birth

Recovery from a CPD-related birth typically extends beyond standard postpartum healing.
Since most cases result in cesarean delivery, physical recovery involves managing surgical pain, gradually increasing activity, and allowing 6-8 weeks for complete healing.
Many women experience emotional challenges, including processing an unexpected birth outcome, potential disappointment, or even trauma from a difficult labor followed by emergency surgery. These feelings may require professional support.
Follow-up care should address both surgical recovery and emotional well-being, with providers monitoring for infection, evaluating incision healing, screening for postpartum depression, and discussing implications for future pregnancies.
A comprehensive recovery plan addresses both physical healing and emotional processing.
Future Pregnancies After CPD

While the recurrence risk for cephalopelvic disproportion (CPD) exists, studies show over 65% of women with prior CPD achieve successful vaginal deliveries in subsequent pregnancies.
Recurrence likelihood increases with fetal macrosomia, gestational diabetes, or post-term pregnancies.
Careful planning involves discussing delivery options (VBAC or cesarean) with a provider, assessing prior labor patterns, fetal size, and pelvic anatomy.
Monitoring maternal health (e.g., blood sugar control) and fetal growth is crucial for reducing risks.
Preventive strategies:
- Manage gestational diabetes rigorously to prevent macrosomia
- Induce labor for post-term pregnancies to avoid excessive fetal growth
- Opt for elective cesarean if prior risk factors (e.g., macrosomia) persist
- Prioritize preconception health (weight management, nutrition) to optimize outcomes
- Supporting Someone Experiencing CPD

For partners and family members, offering emotional reassurance and active presence during medical discussions is vital.
Help them with care decision-making by encouraging open communication with healthcare providers to clarify concerns and options. Collaborating with the care team ensures a unified approach.
Seek resources like prenatal educators, counseling, or support groups (available through hospitals or community organizations) to provide information and emotional relief.
Bringing It All Together
Understanding cephalopelvic disproportion (CPD) is essential for expectant parents going through childbirth. Remember that CPD is identifiable through prenatal measurements, medical history assessment, and progress monitoring during labor.
While CPD may necessitate a cesarean delivery, early detection and proper management ensure positive outcomes for both mother and baby.
Modern obstetric care has significantly improved the safety of C-sections when they become necessary. Most importantly, maintain open communication with your healthcare team.
Ask questions about your pelvic measurements, discuss any concerns about your baby’s size, and explore all available options tailored to your unique situation.
With proper medical care and informed decision-making, families facing CPD can still experience safe, positive birth experiences.
Your birth story may take an unexpected turn, but the destination—a healthy baby and mother—remains the same.
If you’re interested in more informational content on pregnancy, feel free to CLICK HERE and explore other blogs that you might enjoy.

