Ever wondered why your body doesn’t collapse like a ragdoll when you’re standing still? The secret lies in muscle tone—nature’s invisible support system that keeps us balanced and ready for action.
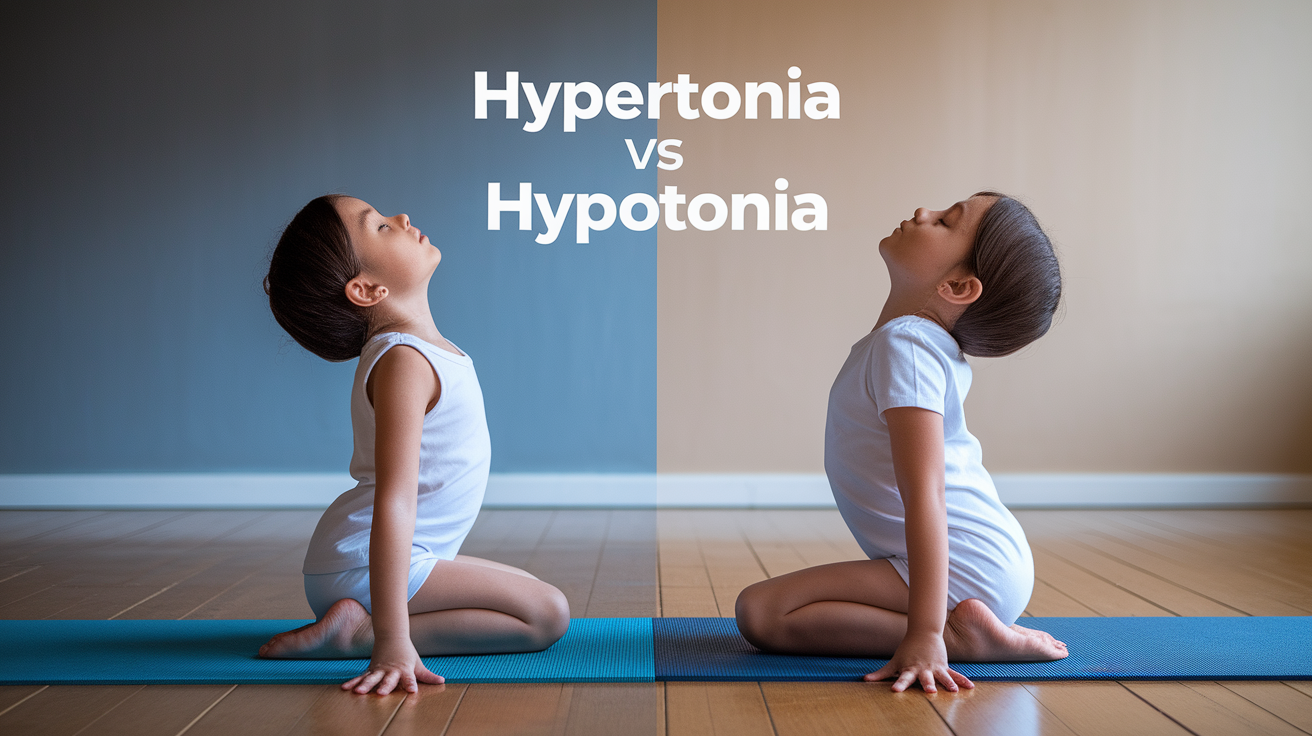
Muscle tone exists on a spectrum, with two notable extremes: hypertonia and hypotonia. Hypertonia refers to abnormally high muscle tone, resulting in stiffness and restricted movement.
At the opposite end, hypotonia occurs when muscles have reduced tension, resulting in a floppy and unstable appearance.
Did you know that newborn babies naturally have higher muscle tone in their flexor muscles? This explains why they often keep their arms and legs curled up—a remnant of their cramped quarters in the womb.
In the following sections, we’ll explore the causes behind these muscle tone imbalances, recognize their symptoms, and find effective treatments to restore your body’s natural equilibrium.
What Is a Muscle Tone?
Muscle tone refers to the constant, low-level contraction of muscles even when they are at rest. This baseline tension keeps muscles ready for action and supports posture without conscious effort.
In normal muscle tone, muscles feel firm yet pliable when relaxed. They respond appropriately to movement demands, neither too rigid nor too floppy. This optimal tension allows for smooth, coordinated movements.
Abnormal muscle tone manifests as either hypertonia (excessive tension) or hypotonia (insufficient tension). Hypertonia causes stiffness and resistance to movement, as observed in conditions such as cerebral palsy or stroke. Hypotonia causes floppiness and instability, often present in certain neuromuscular disorders.
Proper muscle tone is crucial for everyday functions, from maintaining an upright posture to executing precise movements. Without it, even simple tasks become challenging.
What Is Hypertonia?

Hypertonia is a condition characterized by abnormally increased muscle tone, resulting in stiff, rigid muscles with excessive tension and resistance to stretch.
It commonly occurs due to damage to the central nervous system from conditions like cerebral palsy, stroke, traumatic brain injury, multiple sclerosis, or spinal cord injury.
Patients typically experience muscle stiffness, involuntary spasms, abnormal posture, limited range of motion, and difficulty with coordination and fine motor skills. These symptoms can significantly impact daily activities and quality of life.
Treatment approaches include physical therapy, medications such as muscle relaxants, injections like Botox, orthotics, and, in some cases, surgical interventions. Early intervention and consistent management are crucial for improving outcomes and functionality in individuals with hypertonia.
What Is Hypotonia?

Hypotonia, commonly referred to as decreased muscle tone, is a condition characterized by muscles that have reduced tension or resistance to movement.
It typically presents as floppiness, causing affected individuals to appear overly flexible or “floppy”.
The condition often stems from underlying issues affecting the neural pathways or muscles themselves, including genetic disorders (such as Down syndrome, Prader-Willi syndrome), neurological conditions, muscle diseases, or injuries to the brain or spinal cord.
Signs include delayed motor milestones, weak reflexes, difficulty maintaining posture, and a distinctive “rag doll” feel when held.
While some cases improve with time and targeted interventions, others may require ongoing management through physical therapy, occupational therapy, and specialized medical care to maximize mobility and function.
Hypertonia vs Hypotonia: Key Differences
Muscle tone disorders affect millions worldwide, impacting movement and quality of life. This comparison highlights the essential differences between high muscle tone (hypertonia) and low muscle tone (hypotonia).
| FEATURE | HYPERTONIA | HYPOTONIA |
|---|---|---|
| Muscle tone level | Abnormally high muscle tone causing stiffness and rigidity | Abnormally low muscle tone leading to floppiness and reduced resistance |
| Common signs | Tight muscles, limited range of motion, jerky movements, muscle spasms, clenched fist, pointed toes. | Floppy muscles, excessive flexibility, poor posture, delayed motor skills, difficulty maintaining positions |
| Movement effects | Difficulty with smooth movements, coordination problems, abnormal walking patterns | Reduced strength, fatigue during activity, poor stability, and delayed development of motor skills |
| Associated conditions | Cerebral palsy, stroke, multiple sclerosis, traumatic brain injury, Parkinson’s disease | Down syndrome, muscular dystrophy, cerebral palsy, autism spectrum disorders, Prader-Willi syndrome |
| Treatment approaches | Physical therapy, muscle relaxants, botulinum toxin injections, stretching exercises, bracing | Physical therapy, occupational therapy, strength training, adaptive equipment, orthotics |
Understanding these differences enables healthcare providers to develop targeted treatment plans and provides families with insight into managing these conditions effectively.
Causes and Risk Factors
Autism and ADHD share overlapping neurobiological foundations, involving atypical brain development and connectivity in regions governing attention, social cognition, and executive function.
Genetic factors play a significant role, with hundreds of implicated genes affecting neurotransmitter systems and neuronal migration.
Prenatal exposure to environmental toxins, maternal infections, extreme stress, and certain medications increases risk, as do pregnancy and birth complications like premature delivery, low birth weight, and oxygen deprivation.
Early developmental markers may include delayed motor milestones, atypical sensory responses, and differences in joint attention or communication patterns.
Though these conditions have distinct presentations, their shared risk factors suggest common underlying neurodevelopmental pathways, highlighting the importance of early screening in high-risk populations.
Diagnosis and Assessment

Proper diagnosis of muscle tone disorders requires comprehensive assessment techniques and specialized medical expertise. Healthcare professionals utilize systematic approaches to evaluate patients’ motor function and identify underlying neurological conditions.
1. How Doctors Evaluate Muscle Tone
Neurologists assess muscle tone through physical examinations, including passive movement tests and observation of resistance to movement.
They watch for abnormalities during basic movements and may conduct reflex tests to identify conditions of hypertonia or hypotonia.
2. Tests and Tools Used for Diagnosis
Doctors employ various diagnostic tools, including the Modified Ashworth Scale to quantify spasticity and electromyography (EMG) to measure electrical activity in muscles.
Advanced imaging techniques, such as MRI or CT scans, aid in visualizing structural issues that impact muscle function.
3. Importance of Early Detection
Early identification of muscle tone disorders is crucial for effective intervention, particularly in infants and children, as developmental windows are critical during this stage of development.
Prompt diagnosis enables the development of treatment plans, which can significantly improve outcomes and prevent secondary complications.
Treatment Options for Each Condition

Effective management of neurological conditions requires a personalized approach combining therapeutic interventions, medications, and supportive devices. The right treatment plan addresses both symptom management and quality of life considerations.
1. Physical and Occupational Therapy
Physical therapy focuses on improving mobility, strength, and range of motion through targeted exercises. These treatments are customized to address specific motor deficits and prevent contractures.
Occupational therapy helps patients develop the skills necessary for daily activities and increased independence. Therapists may use constraint-induced movement therapy to strengthen muscles that are weakened or paralyzed.
2. Medications
Muscle relaxants, such as baclofen and diazepam, effectively reduce spasticity and improve comfort. Botulinum toxin injections provide localized relief for severe muscle tightness in specific areas.
For seizure management, anticonvulsants are prescribed based on seizure type and frequency.
3. Assistive Devices and Home Care
Mobility aids range from walkers and wheelchairs to refined computer interfaces for communication and interaction. Adaptive equipment transforms living spaces into accessible environments.
Home care services provide essential support for families managing daily care needs.
4. Prognosis and Long-term Management
With early intervention and consistent therapy, many patients show significant improvement. Regular monitoring and adjusting treatment plans as needs change ensure optimal outcomes.
Lifelong management focuses on maximizing independence and quality of life through multidisciplinary approaches.
Living with Hypertonia or Hypotonia
Living with muscle tone disorders presents unique challenges requiring specialized care approaches and consistent support. While hypertonia involves excessive tension and stiffness, hypotonia manifests as decreased muscle tone; both conditions require targeted strategies to enhance quality of life.
Caregivers need patience and specialized knowledge. Daily stretching helps alleviate hypertonia, while strengthening activities benefit individuals with hypotonia.
Adaptive equipment and consistent home therapy routines can significantly enhance comfort and functionality.
Connect with organizations like the Cerebral Palsy Foundation for condition-specific guidance and support. Online and local support groups provide emotional support and practical advice for navigating healthcare challenges.
Early intervention services are essential for development. Collaborate with schools on developing appropriate IEPs or 504 plans that address physical accommodations. Therapy services within schools help build skills for classroom success and independence.
When to See a Specialist
Parents should remain vigilant for certain warning signs that may indicate a need for specialized care.
These include persistent developmental delays, regression in skills, unusual social behaviors, extreme sensory sensitivities, and repetitive movements or behaviors that interfere with daily functioning.
If your child shows limited or no response to their name, lacks eye contact, or has delayed speech development beyond typical milestones, consider seeking professional evaluation. Frequent meltdowns that cannot be explained by typical childhood behavior may also warrant attention.
Early consultation with pediatricians and neurologists is crucial as they can provide comprehensive assessments and appropriate referrals.
Remember that early intervention often leads to better outcomes, so trust your instincts if you feel something isn’t right with your child’s development.
Final Words
Hypertonia and hypotonia represent opposite ends of the muscle tone spectrum. While hypertonia involves excessive muscle tension with rigid, stiff movements, hypotonia presents with decreased muscle tone, causing floppiness and weakness.
The causes differ significantly—hypertonia often stems from brain or spinal cord injuries, while hypotonia may result from genetic disorders, nervous system conditions, or muscle diseases.
Both situations require distinct treatment approaches, with hypertonia benefiting from muscle relaxants and stretching, while hypotonia typically needs strengthening exercises and physical therapy.
Early intervention is crucial for both conditions. Seeking medical help at the first sign of abnormal muscle tone can significantly improve outcomes and quality of life.
Regular follow-up appointments allow healthcare providers to adjust treatment plans as needed, ensuring optimal development and function.
Change muscle challenges into successes! Click here for health-related blogs. Your journey to better movement starts now!

